This post is a detailed explanation of the animated back pain video.
Back pain (AS-type)
Ankylosing spondylitis (AS) is a common type of spondyloarthropathy which causes inflammation of the spine, typically resulting in chronic back stiffness and pain. Individuals carrying the HLA-B27 gene are at high risk of AS-type back pain.

Back pain in men (AS-type)
For a long time, the prevailing consensus was that AS affects only men, because AS inflammation spreads from the prostate to the spine via lymph vessels… and women don’t have prostates! Doctors later realized that spondyloarthropathies affect women’s spine as well, but the symptoms are somewhat different: in women, back pain is typically less severe as compared to peripheral symptoms, and it tends to affect different parts of the spine.
Recent studies indicate that an intracellular fungal infection is present in the prostate (Stott-Miller et al 2013; Sutcliffe et al 2014), and plays an important role in spondyloarthropathies (Laurence et al 2018). The main mechanism of AS-type lower back pain in men is thus:
The human immune system sends T cells to patrol the body, looking for bacterial or fungal proteins which indicate that an infection is present.
A T cell in the prostate spots a fungal protein within a human cell: a fungus is hiding there!
The T cell decides to look for other human cells infected with the same fungus.
The T cell exits the prostate and enters a lymph vessel.
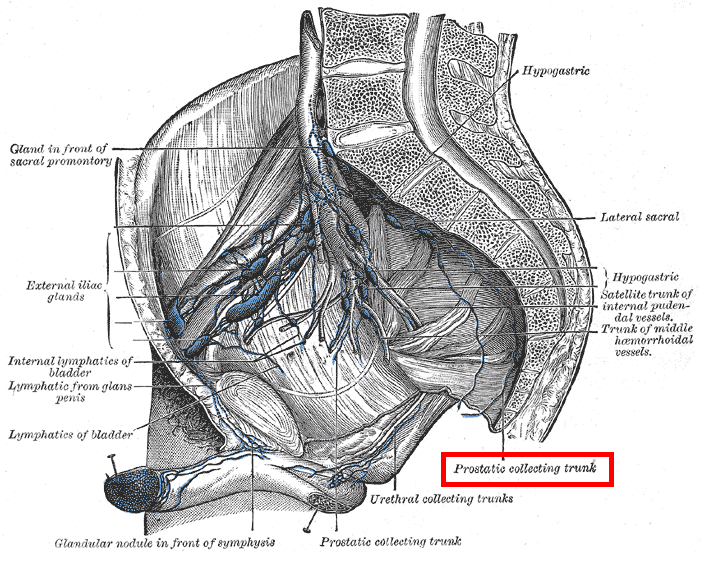
This lymph vessel leads the T cell to the sacroiliac joints, which are located in the lower back, just above the hip bone, on each side of the spine.
The T cell detects the same fungal protein in the sacroiliac joints.
The T cell decides to patrol the sacroiliac joints and spine, killing human cells of the lower back which are infected with this fungus. This causes lower back pain.
In men who do not carry the HLA-B27 gene, detection of this fungal infection by T cells is less efficient, which means it remains largely invisible to the immune system in the prostate and lower back. Note that the fungus is also present in these men, but it causes few symptoms because T cells leave it alone.
Prostate massages cause acute anterior uveitis
The prostate is also involved in reactive arthritis, a well studied type of HLA-B27 spondyloarthropathy where back pain is less severe, but acute anterior uveitis (AAU) often affects the eye. Reactive arthritis can be triggered by massaging the prostate:
“It used to be said of the older venereologists that unless they could produce a flare-up of [reactive arthritis] by prostatic massage they were considered off form. Nowadays, we have either lost this art or perhaps most of us would not care to put it to a test!” (Csonka 1965)
In genetically susceptible individuals, AAU flares-up within a day of prostate massages. Such massages likely push into circulation T cells which are looking for a fungal protein. When these T cells reach the eye, they detect the fungal protein there, causing AAU.
Vedolizumab studies suggest Malassezia is the causative fungus
Crohn’s disease patients who take the drug vedolizumab often suffer from lower back pain as a side effect. This occurs in both sexes, likely because T cells which recognize fungal proteins in the gut are forced to enter other organs (including the spine). This indicates that a fungus must be present in the spine of both men and women, and is the main cause of AS-type back pain in both sexes. Many studies point to Malassezia as being the causative fungus (see here for details).
Back pain in women (AS-type)
Lower back pain in women during menses is very common, and is widely considered unrelated to spondyloarthropathies. This is at least partly wrong.
Women who suffer from spondyloarthropathies don’t have prostates, so T cells which detect Malassezia in their spine must originate from somewhere else! Spondyloarthropathy symptoms in women include chronic inflammation of the cervix, which means Malassezia are very likely present in the uterus. HLA-B27 is expressed there—though less than in the prostate—facilitating the detection Malassezia by T cells.
Lymph vessels which drain the uterus transport T cells to the sacroiliac joints (near the top of the hip bone) and to the para-aortic nodes (a few inches above the hip bone) of the lower back (Hahn et al 1963). This means the seven steps leading to AS-type back pain in men likely also occur in some women, but can affect two regions of the lower back instead of just the sacroiliac joints.


Other menstrual spondyloarthropathies in women
While lower back pain during menses could have myriad different causes (such as referred pain due to uterus contractions), other spondyloarthropathy symptoms which flare-up during menses are much harder to explain. Often, hormones levels in circulation are offered as an explanation, without any strong supporting mechanistic evidence.
AAU is a very specific spondyloarthropathy symptom of the eye caused by T cells, and is not explicable by referred menstrual pain. AAU flare-up risk is much higher near menses (Sanghvi et al 2004). The simplest explanation for this phenomenon is that the uterus is cyclically producing T cells which recognize Malassezia. These T cells then enter circulation and search for Malassezia in all organs of the body, including the eye. This process is very similar to prostate massages in men, except it happens naturally at the end of each menstrual cycle (McDonagh et al 1993; Salamonsen et al 2000).
Other spondyloarthropathy-associated symptoms that have been reported to flare-up in association with menses include inflammatory bowel disease (Kane et al 1998) and psoriasis (Stevens et al 1993). T cells recognizing Malassezia proteins are causative in both (see here for details).
Summary
Differences in lymphatic drainage between genital organs (prostate / uterus) can explain why ankylosing spondylitis is more common and severe in men, and why lower back pain in women during menses affects the para-aortic region (a few inches above the hip bone) in addition to the sacroiliac region (near the top of the hip bone). Menstrual spondyloarthropathy symptoms such as AAU indicate that T cells which detect Malassezia proteins are produced during menses. This means menses-associated lower back pain is at least partly due to Malassezia in the spine being attacked by T cells which activated in the uterus.
NB: This post is based on Laurence et al 2018 (simplified for clarity). While many cases of back pain are the results of spondyloarthropathies, others are due to physical trauma, spinal disc herniation, etc.
Animated back pain (AS) video (intro): https://youtu.be/S-VhDiqwBnk
Animated back pain (AS) video (full): https://youtu.be/e2vpMqmLYQo

Comments